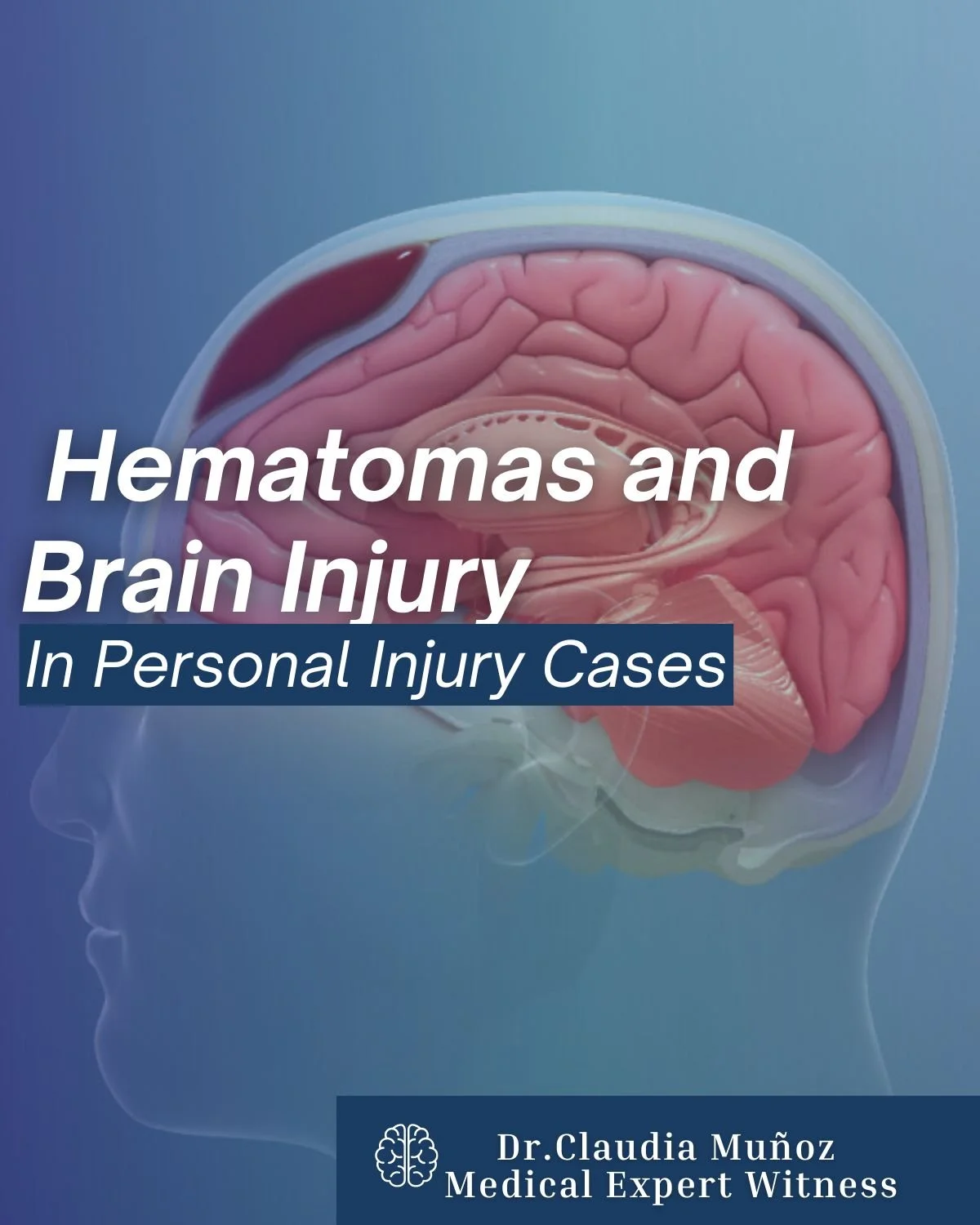
Hematomas After Head Trauma: Legal Perspectives
A hematoma following head trauma may not be visible immediately, but it can rapidly become one of the most dangerous complications of a brain injury.
As a Neurologist and Medical Expert Witness, I’ve seen how crucial it is to recognize the subtle signs early and understand the full neurological impact behind them.
What Is a Hematoma?
A hematoma is a collection of blood that forms outside of blood vessels, often as a result of trauma. When it occurs inside the skull, it can compress brain tissue and interfere with normal brain function. Even a small bleed can cause significant neurological consequences, particularly when pressure builds within the skull, a condition known as increased intracranial pressure (ICP). Depending on the location, we classify hematomas as:
Epidural hematoma – bleeding between the skull and the dura mater.
Subdural hematoma – bleeding beneath the dura mater, usually from veins
Intracerebral hematoma – bleeding directly within brain tissue.
Not all hematomas appear right after impact. Symptoms may develop hours or even days later, which can lead to dangerous delays in diagnosis.
In both clinical and legal settings, understanding when and how the hematoma formed is critical. Important points are:
Timing helps correlate neurological decline with the original trauma.
Mechanism clarifies whether the bleeding pattern matches the reported event or suggests alternative causes.
Progression determines if the injury was aggravated by delayed medical care or secondary impacts.
This level of detail is often pivotal not only for treatment decisions but also for establishing causation and liability in personal injury or defense cases.
Neurological Evaluation and Diagnosis
Prompt neurological evaluation can be life-saving. Neuroimaging — such as CT or MRI — allows us to visualize bleeding, monitor expansion, and determine whether surgical intervention is required.
In expert witness work, objective evidence from imaging, clinical notes, and neuropsychological assessments helps establish the extent of injury and its impact on cognition, behavior, and daily function.
Bridging medicine and law requires clarity, precision, and neutrality. An accurate, evidence-based neurological evaluation ensures that both medical and legal decisions are grounded in objective science — not speculation.
As a Medical Expert Witness, my role is to interpret neurological findings, explain them in clear terms, and provide defensible medical opinions that support fair outcomes for all parties involved.
A hematoma is more than a simple bruise — it’s a dynamic and potentially life-threatening event that demands timely recognition, accurate evaluation, and expert interpretation.
By combining clinical expertise with clear communication, neurologists can play a key role in improving patient recovery and ensuring justice in cases where brain injury is involved.
Connect for Expert Support
If you handle personal injury or defense cases, I offer neurological evaluations, expert testimony, and case reviews grounded in medical accuracy and clarity.
📩 For inquiries or consultations: doctor.claudia@gmail.com